10 december 2020 – First use Inreda AP in the east of the Netherlands
Dear reader,
Welcome to the third news letter of 2020.
We have good news: the first Inreda AP’s are in use now. Our first step in the market has been taken. We have started a first project with a small group of adults with type 1 diabetes in a few hospitals in the east of the Netherlands. It is a partnership between Inreda, the hospitals and health insurer Menzis. Read on at the first item First use of the Inreda AP.
We are also working on new studies. For example, a study with people whose pancreas has been removed. Immediately after removal, these people have diabetes, also called type 3. How are these people doing when they use the Inreda AP? We will tell you more about this in Study Inreda AP in type 3 diabetes.
Finally, one of our colleagues will be put in the spotlight and tell you a little bit about herself. This time, it is the one who is responsible for everything that has to do with the medical side. You will find this under the last item: Colleague in the Spotlight.
Enjoy reading!
Team Inreda
First use of the Inreda AP
Working together with health insurer Menzis
After having achieved CE marking, we take the first step in the market by having a group of people in the east of the Netherlands who are insured with Menzis use the Inreda AP. In this project with Menzis, the first adult people with type 1 diabetes will start with the AP treatment, Then, more people will follow step by step. With this project, we want to initiate large-scale production and sales to as many people as possible. The latter can be better achieved if the artificial pancreas is included in the health insurance. If it has been proven that the Inreda AP does what it should do. Even with larger numbers of patients, the system can be used more widely. We assume that the Inreda AP has proven its added value and is eligible for reimbursement. With this project, we want to show that this is possible. Robin Koops: “Ultimately, that is the dream of many ‘diabetes people’. Improve our lives and regain our freedom. That is now reality!”

Health insurer Menzis was immediately enthusiastic about the Inreda AP and was prepared to invest in the interests of its policyholders. Ruben Wenselaar, Chairman of the Board of Directors at Menzis: “We are happy to contribute to innovative projects that add value to the quality of care for our policyholders. We were immediately enthusiastic about the Inreda AP. With this innovative device you can make life a lot more comfortable for a large group of chronically ill people. That is in line with our mission in which, in addition to good, accessible and affordable care, we also consider strengthening the vitality of every person to be important.”
Hospitals and medical support
A number of hospitals in the provinces of Gelderland and Overijssel in the Netherlands are participating in this project: Rijnstate Hospital (Arnhem), Slingeland Hospital (Doetinchem), Canisius Wilhelmina Hospital (Nijmegen), Gelderse Vallei Hospital (Ede), Hospital Group Twente (Almelo) and Medisch Spectrum Twente (Enschede).
The treating physician and diabetes nurse remain the medical contact for diabetes treatment. It is very important that there is and remains good contact between the patient and the treatment team.

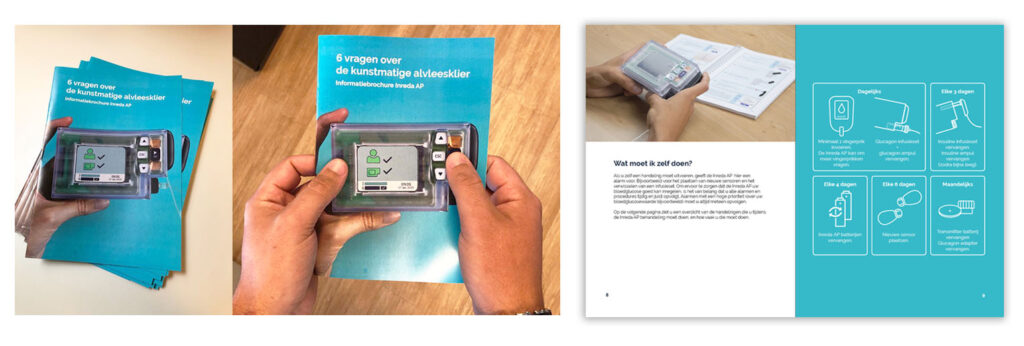
First trainings
Prior to the start of the AP treatment, the patients are trained for two days. For the time being this takes place in the cultural center of Goor. A training center has been set up here to properly prepare patients for the AP treatment. We do this to quickly familiarize the users with the new system. During the training, people get to know the device well. The Inreda AP is put into use on the second day.
Voorafgaand aan de start van de AP behandeling, worden de patiënten twee dagen getraind; vooralsnog vindt dit plaats in het cultureel centrum van Goor. Hier is een trainingscentrum ingericht om de patiënten goed voor te bereiden op de AP behandeling. Dit doen wij om de gebruikers snel vertrouwd te laten raken met het nieuwe systeem. Tijdens de training leren de mensen het apparaat goed kennen en wordt op de tweede dag de Inreda AP in gebruik genomen.
24-hour telephone accessibility
After the training days, people have various contact moments with their personal coach from Inreda. Inreda also offers aftercare via a Customer Service, a 24-hour telephone accessibility to quickly provide the right solution in case of problems.

Inreda AP study in type 3 diabetes
In this study, in which Inreda collaborated with the Amsterdam UMC, research was conducted on people who developed diabetes because their pancreas was removed (also called type 3). In this study, which aims to investigate the effect of treatment with the AP on glucose regulation, 12 people with type 3 diabetes used the Inreda AP.
The study consisted of a feasibility phase and the main study. The feasibility phase took place at the beginning of September. This test period was used to improve study procedures, among other things. In this phase, two participants used the Inreda AP for five days and this went well.
The main study consisted of a control part in which the participants used their own insulin treatment in combination with a blinded sensor (open loop period), and the artificial pancreas part in which the participants received the AP treatment for a period of 1 week (closed loop period). Half of the participants started the main study with the open loop period followed by the AP treatment, and for the other half of the participants this was the other way around.
The closed loop period of the main study was successfully completed in October by ten study participants. The responses from the participants were mixed. The participants were positive and enthusiastic about the improvements in glucose control. However, daily use of the Inreda AP turned out to be more work than expected for some participants.
In the meantime, the participants have also completed the final control part of the study and the first analyses are taking place. If more official results are known, we hope to be able to mention them in one of the following newsletters.
Colleague in the Spotlight

Who are you?
I am Helga Blauw. I am 33 years old, I live with Enno in Twello and have a sweet 2.5 year old son Noan. I studied Technical Medicine at the University of Twente in Enschede. After that, I could immediately start working at Inreda. I have been working there for more than 8 years, since October 2012. After graduating, I also started doing my PhD research at the Amsterdam UMC, location AMC. I hope to obtain my PhD around May 2021.
What do you do?
II am responsible for the medical department of Inreda, which now employs 6 people. We are a young department with many young people. We conduct the clinical examinations and, where necessary, offer medical guidance to the users of the Inreda AP. We also offer medical expertise to, for example, the R&D department, for the development of the artificial pancreas. Medical ensures sufficient safety and quality of the device; this is supported by clinical data. We keep an eye on the state of the art: what is going on in the field of diabetes and we take that into account when developing the device.
Do you have a passion for something?
My motivation is to connect the medical and technical world. Building a bridge between those two worlds. I think it’s fantastic when the device is fully used in clinical practice. From the medical side of Inreda and as a team, I would like to mean even more and achieve more. Also expand my team further and ensure that we function optimally as a team. My ultimate goal is that with the Inreda AP we reach as many people as possible who can benefit from this treatment, including children and other adult groups. We want to use the feedback derived from the practical experience that we are going to gain with various user groups, so that we can use that input to further improve the device.
What do you do in your free time?
In normal times I play volleyball – competitively, but also for fun. This spring I started baking, and now in the “second corona wave” I am going to pick up cycling. I also like to do fun things with my son.
How did you get a job at Inreda?
When I was graduating, I saw a vacancy from Inreda through my study program. I called and was then allowed to come for an interview. That first meeting was with Robin Koops and Hans de Vries (then an internist, now a professor of internal medicine at Amsterdam UMC, location AMC). After that conversation I was immediately called back when I was on the train back home: I could get started. My assignment was to minimize the artificial pancreas from laptop size to pocket size; I also started the clinical studies with the reduced prototype. That was also the immediate start of my PhD program at the AMC. Inreda, the AMC and a few other project partners received a European subsidy in 2012 with which we could do the development and the clinical studies.
Has something fun, crazy or memorable happened at work?
I really enjoy looking back on those 8 years of development. When I started in 2012, Inreda was still in its infancy, with a very small office and, next to Robin Koops and other friends involved, one employee, that was me. From that very beginning until now I have been moved forward from place to place, literally but also figuratively. We have grown tremendously, together. We can all be extremely proud of that, that we have come this far despite some setbacks along the way.
What do you do in 5 years time? What is your goal?
I hope that the medical department will be a lot bigger and that we can do many studies at the same time to be able to test all further developments. And that we can also conduct European studies and research when we enter the market in other countries. This could be, for example, studies for reimbursement in that country or observational studies: how do people and healthcare in that country deal with the Inreda AP. And sometimes professional groups ask for studies, for example into effectiveness. I also find an important question to investigate: how do we implement the artificial pancreas in healthcare? Furthermore, I would like to make the Inreda AP more user-friendly based on the feedback from the projects and studies. And I hope that we can then measure and see the (hopefully positive) health effects in the longer term, where my team then takes care of the coordination of these studies, rather than the measurements themselves.
